At Alliance, it’s all about having personalized health care.
Part of that personalization frequently involves prescription medications.
Knowing the chemistry and genetics of each individual can significantly influence the response to those therapies.
At Alliance, we are literally aiming to hit the mark as close as possible without undue side effects.
Science is finally catching up to modern prescription management and we are pleased to offer our patients pharmacogenomic testing.
The concept is foreign to many, so we thought it worth a short primer:
First, let’s start with WHAT IS pharmacogenomics?
Pharmacogenomics is an important example of precision medicine, which aims to tailor medical treatment to each person or to a group of people. Pharmacogenomics looks at how your DNA affects the way you respond to medications. In some cases, your DNA can affect whether you have a bad reaction to a medicine, whether a medicine helps you, or whether it has no effect. Pharmacogenomics can improve your health by helping you know ahead of time whether a medication is likely to have its’ predicted affect or be more likely to cause side effects.
Next, what does the genetic profile MEAN?
Medications interact with the body in numerous ways. After taking a medicine, the body needs to absorb it, process it, get it to the intended area, and then eliminate the excess and the metabolites. DNA can affect any of these steps and thus influence the response to a given medication. Some examples:
• Drug Receptors. Some medications need to attach to proteins on the surface of cells, called receptors, in order to be absorbed and/or be converted to work properly. Your DNA determines what type of receptors you have and how many, which can affect your response to the medicine. You might need a higher or lower amount of the medication than most people or a different medicine entirely.
• Drug Presence. Your DNA can also affect how quickly some medications are removed from the cells in which they act. If medicines are removed from the cell too quickly, they might not have time to function effectively. If they persist longer than needed, side effects happen.
• Drug Breakdown. Your DNA can affect how quickly your body breaks down and eliminates a medication. If you break the medicine down more quickly than most people, your body gets rid of the medicine faster and you might need more of the medicine or a different medicine. If your body breaks the medication down more slowly, you might need less of the medicine.
• Metabolites. Many medicines get processed into another chemical form, which can also be metabolically active, and which follows its’ own pathway for breakdown and elimination. And then there are the metabolites that interact with one another or with a separate medicine.
Knowing this, test results infer a genetic profile of a specific enzyme that would be consistent with a poor, normal, or rapid metabolizer of medications utilizing that enzyme pathway. To make things even more complicated, someone may be a poor metabolizer via one enzyme, but an extensive metabolizer for another, all involving separate processes followed by the same medication. So complicated.
Doctors will then use this information to better predict which medications may require dose adjustments, may be less likely to work, or may have an increased risk of side effects based on your genetic makeup.
The science is just now catching up with what all doctors knew, that some medicines work for some people and those same medicines don’t work or cause harm to others. Doctors routinely assess benefit/risk of a medication via frequent follow up visits with questions and lab testing. But now, at the time of choosing to medicate, a decision can be made ahead of time. A decision influenced by science, that certain medications may work better with your unique genetic profile, some may be more likely to have side effects, and some might not work at all.
There are several laboratories that offer such testing, though each is different on what they test, how many genes they test, how many meds they cross reference, and how much distillation of the data they provide. It can be overwhelming.
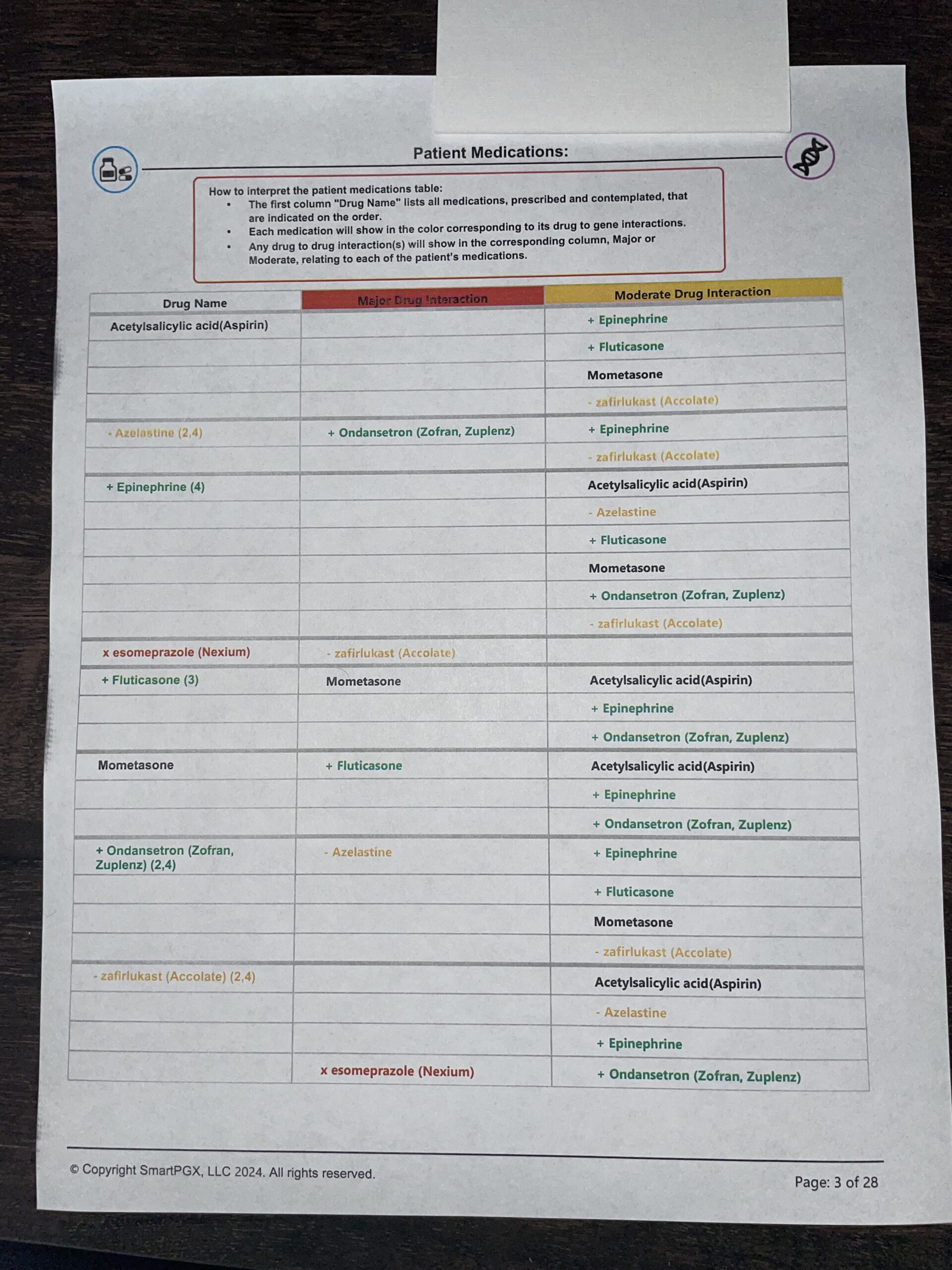
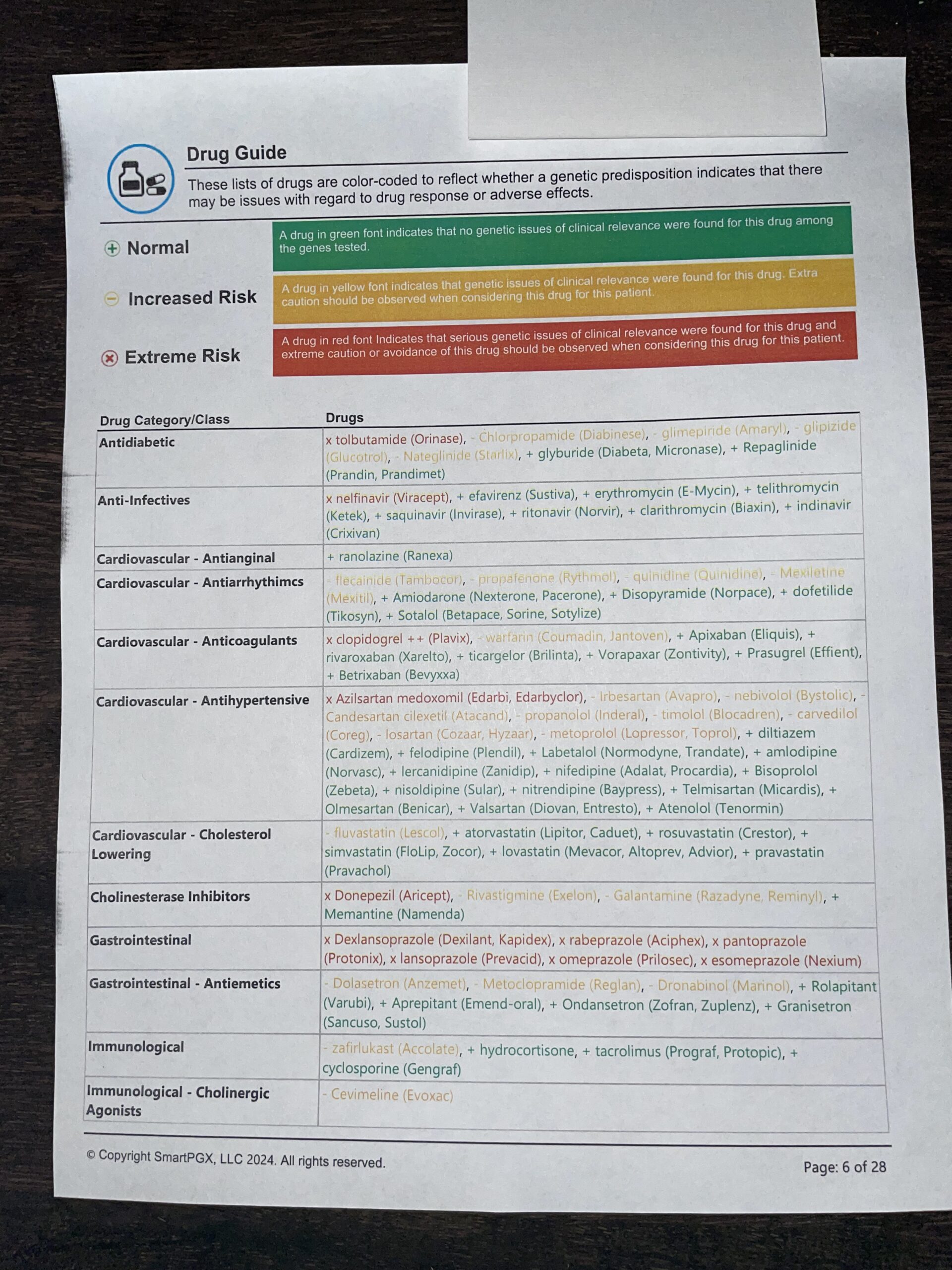
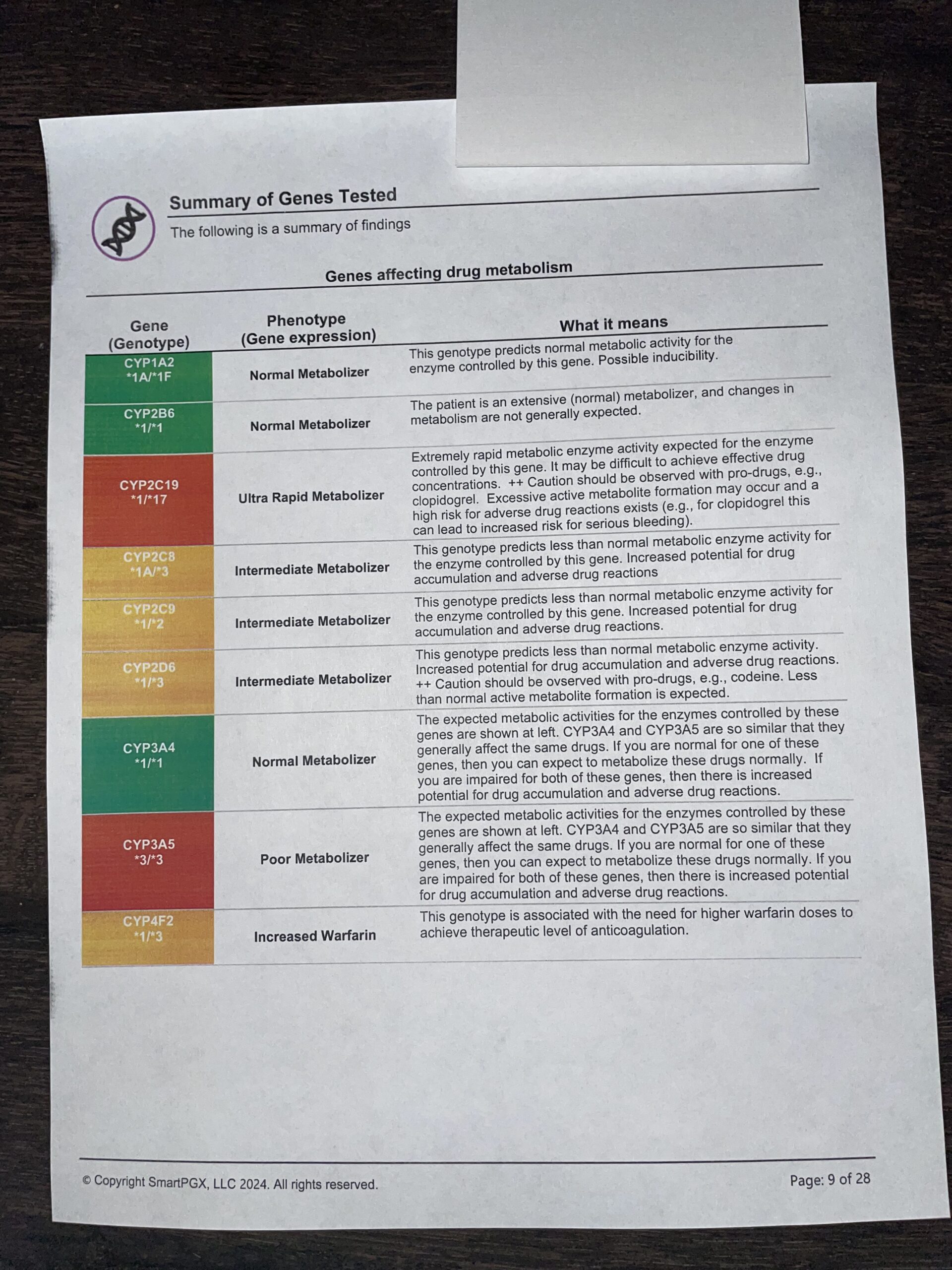
Here is an example of a report that we receive (3 of the 20+ pages):
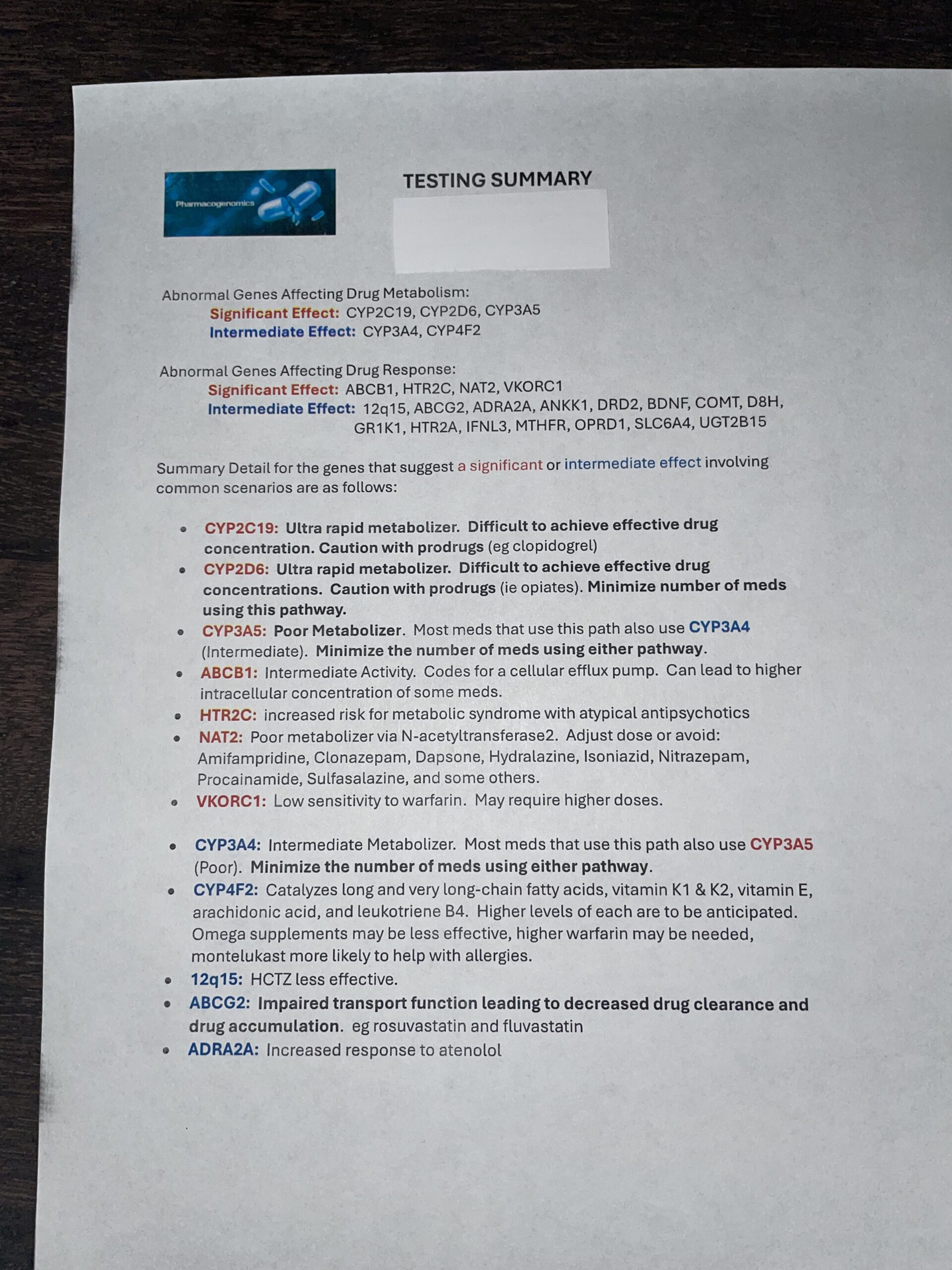
As you can see, it is a lot of data and difficult to summarize, which is what you (the patient) and all doctors, are going to want. That summary can look something like this:
But it still lacks the specifics of what THIS report means TO YOU. That’s where we do our best, using our experience and our pofessional opinion, to distill that data into something specific and meaningful.
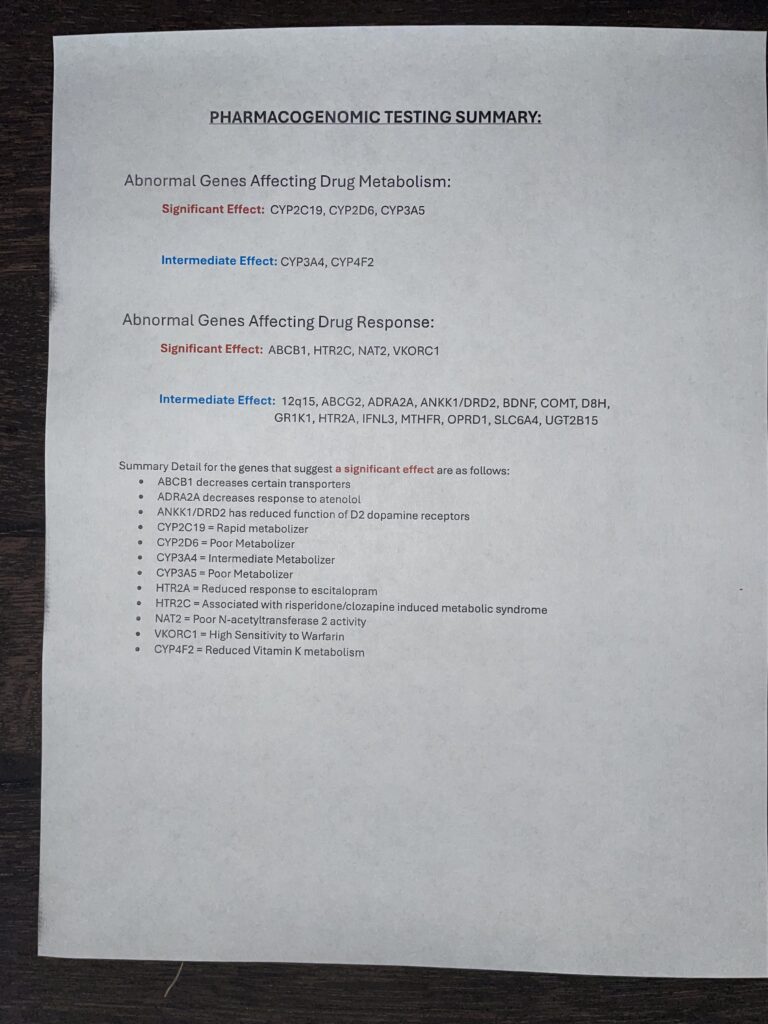
Our summary report will look something like this:
From there, we make a joint decision on whether to change anything or to change a lot of things. Little within these profiles is crystal clear. In fact, at this time it should be considered a dull tool, filled with nebulous suggestions, but we find that it frequently sheds light on why certain meds were not tolerated in the past and it certainly helps to choose meds that are predicted to be metabolized in a normal fashion.
Precision Medicine … Personalized Care … Alliance Personalized Health Care