We venture to say that most patients are familiar with the word cholesterol and have some concept of the importance it plays in cardiovascular health. It is also likely that most people have heard that there is more to it than simply measuring total cholesterol. Afterall, when was the last time your doctor ordered anything other than a four way profile of LDL, HDL, Triglycerides, and Total Cholesterol? And for those of you who like math, did you know the formula (roughly) is: HDL + LDL + 0.2(Triglycerides) = Total ?
It can be helpful to use a real patient scenario. This is the result from someone we will call “Jose”. It looks pretty good on the surface. But it may be helpful if you knew that Jose has a lot of vascular problems. Could there be something within the cholesterol profile to explain things, you may ask. Of course there is! Otherwise, we wouldn’t be having this discussion.

It is already getting complicated. But oh how much more we can learn by breaking down each of those components AND adding some related components not yet discussed. Keep in mind that it is all about vascular health, preventing hardening of the arteries (arteriosclerosis) by preventing clotting of the arteries (atherosclerosis). If you want to learn more, then read on, and we will try to relate a distilled version of what WE know, acknowledging there are others with more advanced understanding of this evolving science called “lipidology”.
Here at Alliance, we recommend that you get your cholesterol checked on a periodic basis, which timeline can vary based on your personal history, family history, and specific risk factors. There are several commercially available advanced tests for cholesterol assessment that will break down the three particles mentioned above and add those other factors that affect vascular health. It may be appropriate to do one of these more advanced tests, based on your personal risk factors and your discussion with your physician. Based on several criteria, we have chosen to work with a product called CardioIQ, offered by QuestLabs (located in the building adjacent to our office).
To get started, let’s talk about LDL (Low Density Lipoprotein), commonly referred to as the “bad cholesterol”. Note how the full name implies it is not a single molecule, rather a merger of lipid (“lipo”) onto a carrier protein (“protein”). Starting with the lipid component, not all low density lipids are the same. When you get a report back indicating that the LDL level is “69” (as in the example above), that does not tell the whole story. Think of that number like naming the size of a jar. A jar of size “69” IS bigger than 50 and smaller than 100, but it’s time to ask what is INSIDE the jar. Two individuals could have the same report of an LDL of 69, which accurately reflects that the volume of LDL IS 69, but if we line up the two same sized jars, they may be completely full of DIFFERENT SIZE lipids. Think of it like jars of candy. Same size jars (that’s the “69”). But inside there is clearly a difference as one jar holds a whole lot more pieces of candy (smaller bites) than the other jar.

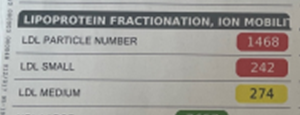
As it turns out, that’s important. The smaller the lipid particles, the easier they penetrate the walls of the arteries. We don’t want them inside the walls, as that sets up atherosclerosis. The advanced lipid profiles will break that down, reporting things like this. The LDL of 69 seemed great (goal for someone with Jose’s condition is <70). But, it is mostly made of small dense particles. That jar holds a lot of them. Maybe Jose should try for an even lower level of LDL.
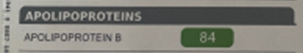
Even then, the story is not complete as the lipid component is bound onto a protein component called apolipoprotein. In the case of LDL, it’s apolipoprotein B, and there are several of them. They are not all the same with regards to atherogenicity. If we stick with the candy analogy, it would be like breaking open two different patients LDL that may appear almost the same on the surface, only to find something different on the inside. Think gumballs.


Let’s stop the discussion at that point. Jose’s report shows that the ApoB level is reasonable. If it wasn’t, then the discussion gets a bit more complicated.
Then, there is HDL, commonly referred to as the “good cholesterol”. The same understanding can be had there. We want the lipid component to be large and we want the apolipoprotein component to NOT be one called “little a” (I know, real original). And the apolipoprotein profile can be broken down further as well. Note how Jose’s report shows a healthy size HDL, reflected in his original decent volume number of 43, BUT the core has a lot of lipoprotein (a), a highly atherogenic particle. It is very hard to treat, though there are meds in clinical trials that offer great promise. Even without the medicine though, it certainly changes how we approach this patient. His cholesterol profile is NOT good.
It helps a lot to move past the cholesterol itself and consider other markers that increase inflammation at and inside the wall of the artery. As we learn more and more, inflammation is at the core of many disease processes. The CardioIQ profile will report a helpful graphic.
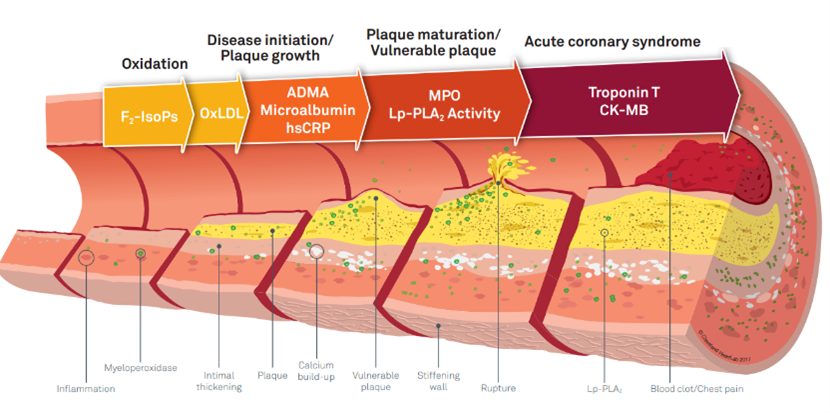
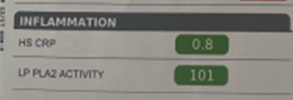
We find it helpful to measure some or all of these markers depending on the clinical situation. They are a mixture of blood and urine tests, that can let us know if there is little active inflammation but highly irritating particles, probable plaque presence, or some evidence for active inflammation (which is more dangerous and which may change the treatment plan). Back to Jose. Here are his inflammatory marker results, and you can see there is some evidence of vulnerable plaque.
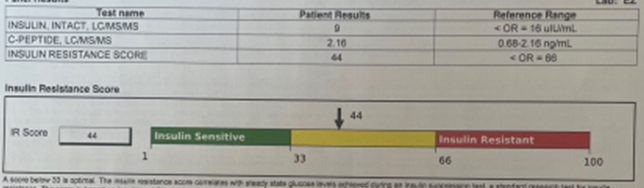
A natural question is to ask what causes such degree of inflammation. The answer is, A LOT OF THINGS, including the size of the lipids, the type of the apolipoproteins, lifestyle choices such as smoking and being sedentary, as well as other disease processes such as diabetes. It turns out the CardioIQ can also check for insulin resistance as well, and here is Jose’s result. Note the educational graphic.
That completes the basic tour of an advanced lipid profile and what can be gained. In the case of Jose, note how much more there is to the story behind what looks like an excellent lipid profile. What did he and his doctor decide to do? Well, we changed the statin, increased the dose, and added two other lipid lowering agents that might affect the lipoproteins and particle numbers. We added an exercise regimen to promote arterial health and lower the glucose, made additional dietary recommendations, emphasized smoking cessation, and we will repeat things in a few months for comparison. We suspect he will be a great candidate for the forthcoming new medications that will treat lipoprotein (a). None of this would be known or likely have been done without the more advanced profile.
Not everyone needs the testing. Sometimes inquiring minds just want to know. All of that is within reason. At Alliance, we want to work WITH you in order to make a joint decision on when to test, what to test, and what to do with the results of that test. It’s good to know what is really out there and available.