Neurocognition refers to the functional aspects of the brain. That includes receiving proper input from the senses (hearing, vision, touch, smell). It involves the processing of received information. It certainly involves the orchestration of complex movements, emotional interactions with others, and complex thought processing.
At Alliance, we believe in screening for problems in this area rather than waiting for symptoms to surface. Neurocognitive decline is far more common than most realize. Here are some facts:
• The prevalence of subjective cognitive decline is 11%, or 1 in 9 adults.
• The prevalence by age breakdown is: age >65 years = 11.7%, age 45-64 years = 10.8%.
• The prevalence by sex breakdown is: 11.3% among men and 10.6% among women.
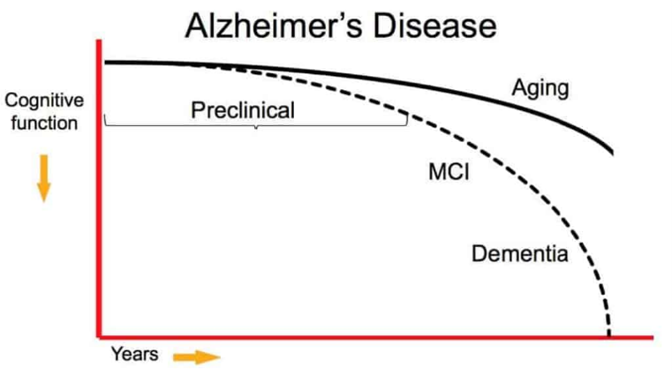
• The prevalence increases steadily with age, so that by age 90, about 33% have dementia.


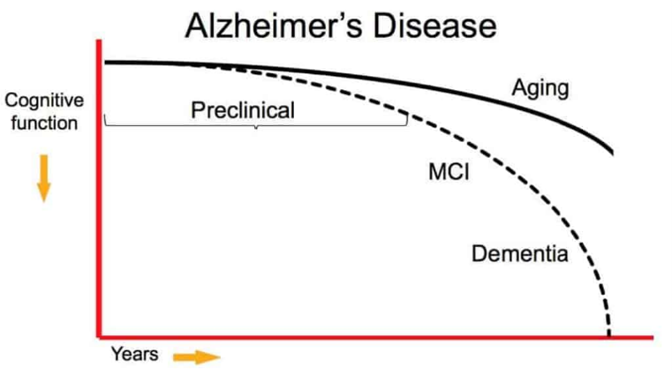
Note how early the decline is reported. So, when we think we are not processing information as fast or our reaction times are not as fast as they were just a few years ago, it may be accurate. It may not be a problem that needs to be fixed, but there are ways to optimize our well being so as to compensate for minor changes. If you are wondering about those early symptoms, here is a graphic.
Adding to the surprise of how early in life decline is noted, is the following:
Less than half of adults with Subjective Cognitive Decline (45.3% of adults aged 45 years and older) reported discussing symptoms of confusion or memory loss with a health care professional.
At Alliance, we won’t wait for you to “bring it up”. We will ask you directly, and then put some science to the subject. And here is a big part of the why:
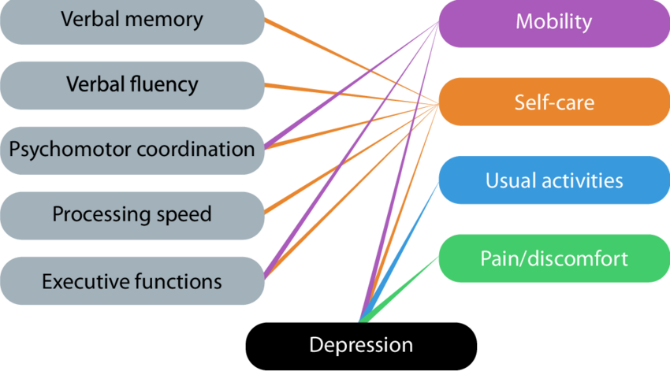
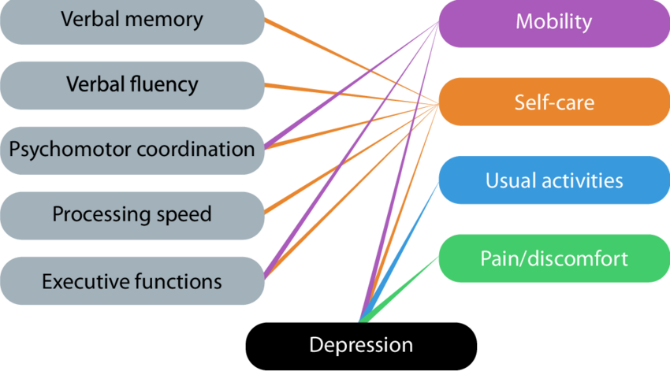
28% (1 in 4) with Subjective Cognitive Decline have coronary heart disease or have had a stroke, 33% (1 in 3) report frequent mental distress, and 66% (2 in 3) have at least two chronic diseases.
So, if a deficit is noted on screening, that’s why such an extensive evaluation begins. It’s to uncover the other things that are going on.
The Basic Screening Tests Done at Alliance
I mentioned screening tests. Here are the tests you can expect on a periodic basis inside our office (perhaps annually after the age of 50):
• Hearing (In office, computer based, 250-8000 Hz, 0-100 dB)

• Vision (typical eyechart or referral to ophthalmology)
• gait/balance assessment (often the BERG test, usually done via visiting physical therapists in our office

• paper based cognitive testing (MOCA/SLUM/MMSE). Either test is administered by medical staff, takes about 10 minutes, and has a 90% sensitivity for detection of early cognitive decline. There are 8-11 questions, scored individually and as a composite, that assess the areas of visuospatial discrimination, executive function, naming, immediate and delayed recall, attention, language, abstraction, and orientation.

• various blood tests

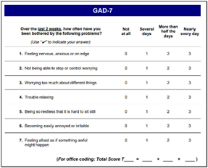
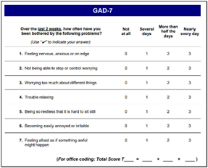
• screening for anxiety (GAD-7). It scores seven criteria for generalized anxiety. It is self-administered and scored as 0-3 in each area. It has over 80% sensitivity and takes about 2 minutes to fill out.
• screening for depression (PHQ-9). It scores nine criteria for major depression. It is self-administered and scored as 0-3 in each area. It has over 80% sensitivity and takes about 3 minutes to fill out.


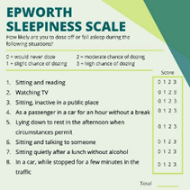
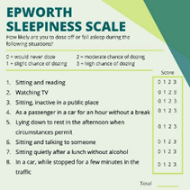
• screening for sleepiness (Epworth Sleepiness Scale). Often overlooked is sleep quality. We use the Epworth Sleepiness Scale, which tests 8 areas for a total score of 0-24. Should a significant problem be noted, then a more intense focus on sleep hygiene or wakefulness promotion can be engaged.
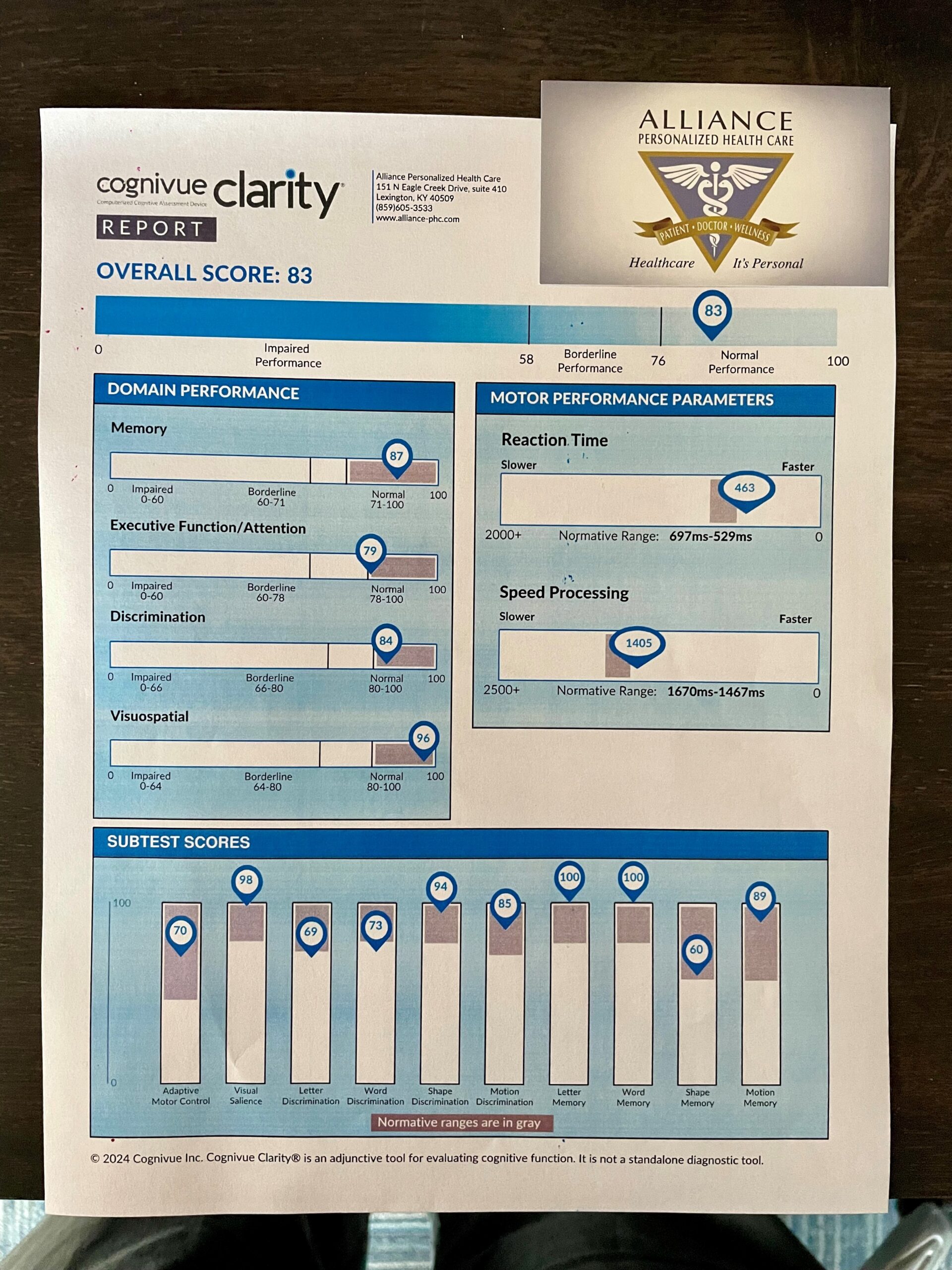
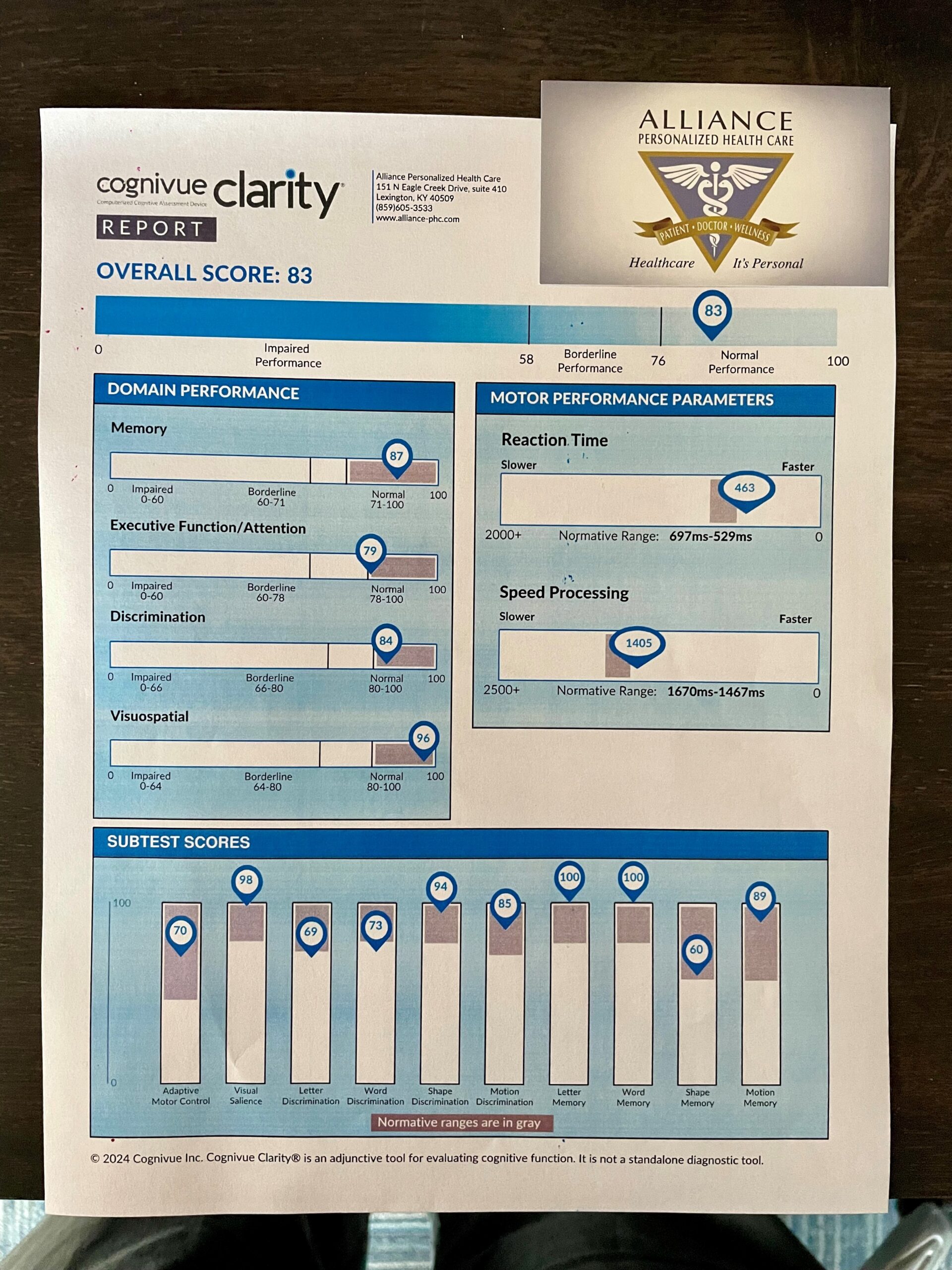
Corelated with memory decline is visual processing of different inputs. Previously, this has been hard to test in a primary care clinic, but such is not the case anymore. We are pleased to have in our office, a device called Cognivue. The test is a self-paced, computerized test that takes 10 minutes. The test uses visual cues and manual responses to assess fine motor skills, basic visual acuity, perception discrimination of letters/words/shapes, and short-term memory of letters/words/shapes/motion. All in all, this adds significantly to the established norms. Supposing that tests return normal, then we will score it, record it in your chart, and then retest in a year.


Workup for Cognitive Decline
If you think that sounds like a lot for generalized screening, take a moment to think how much of your everyday activities involve the brain. Virtually every waking moment AND every sleeping moment. As we know, early detection helps just about everything. Should a deficit be identified, then a plethora of additional tests may be called upon (at which time you won’t think the generalized screening was all that much). These next level tests could involve:
• Pharmacogenomic Testing (genetic testing done in our office of 40+ genes used to metabolize medications). No one has a completely normal test, and it allows for custom medication management.


• Imaging tests of brain, vasculature, and more. This may involve a myriad of choices involving xray, ultrasound, CT, and MRI.


• Extensive blood tests for infection, autoimmune disease, vitamin/mineral deficiencies, hormonal abnormalities, toxicities, and even occult malignancy



• Potential genetic panel testing


• Dietician Consultation in our office


• Sleep Study


• Referral to Psychology


• Referral to Occupational Therapy, Physical Therapy, Neurologist, Neurocognition Specialist and others as indicated.


Helpful in this evaluation process is our access to a panel of tests, which subsequently generate a report for you that is colorful, descriptive, and breaks things down for better understanding. The same test will integrate measurements of p-tau protein, beta-amyloid proteins, and apoE gene testing (all correlated with progressive forms of dementia).
As you can see, things can get quite complicated. But the brain is at the center of everything. Therefore, everything influences its’ function. Understanding how all that interacts and engaging early in the process is why we do these assessments.
Should we encounter a problem, it will likely involve a multimodal approach. We will guide you through what is needed and orient you to valuable resources moving forward. Exactly what will be needed varies. Some things are universal. But we will also focus on YOUR associated medical problems (remember, 66% have multiple other medical problems). Healthcare is not “one size fits all”.




And knowing that most will not have an active issue, there are plenty of proactive interventions to help reduce the risk of one day getting there. Meanwhile, we screen periodically. You worked hard to build the mind that you have; we will work hard to help you keep it.